For people living with long term health conditions, it can be difficult to know whether exercise will help or exacerbate symptoms and the anxiety and confusion around this can prevent them from exercising at all. The truth is, there are very few conditions that exercise is unable to help with, although amendments may need to be made to make sure exercise is safe and effective for each individual and their medical history. Many people may avoid exercise or physical activity in order to prevent short term pain or discomfort or simply through anxiety, however this often makes matters worse. This blog discusses a common long term health condition, arthritis, and how exercise can help to manage it.
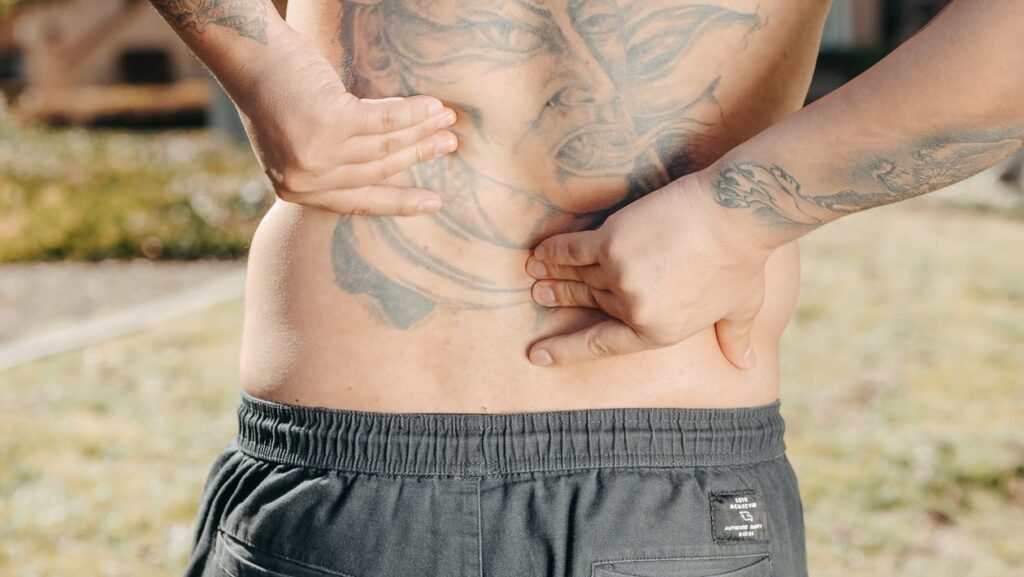
Arthritis affects the joints of the body and whilst there are several different types under this ‘umbrella’ term, this blog discusses the most common of these. Osteoarthritis is a degenerative condition of the joints that is most commonly brought on by the natural wear and tear associated with daily living and movement. The cartilage in affected joints becomes worn down, making movement at the joints more difficult and often painful. The outer edges of bones can thicken and change shape and bony growths form at the outer edges. As a result of all this the joints can become inflamed and swollen. In some cases, calcification occurs hardening joints further. The primary joints affected are the weight bearing joints of the body such as knees, hips, the lumbar spine, wrists and hands.
Osteoarthritis is more common in men before the age of 45 and women after the age of 45. This may be to do with higher participation in sports by men or more specifically the nature of many sports that generally more male-dominated such as rugby, football and boxing. There may be other factors involved, however, and whilst the causes of osteoarthritis aren’t fully known there are some widely agreed contributory factors:
The natural ageing process and the culmination of years of wear and tear is a primary cause and risk factor, although osteoarthritis can also occur in younger age groups.
Being overweight increases the stress placed on joints and can contribute to deterioration. The more overweight a person is, the greater the strain on joints.
Injury to joints can make them more susceptible to wear and tear and/or osteoarthritis, therefore athletes or highly active people can be at higher risk.
Overuse of joints such as overly repetitive movements or positions through sports or occupation may be a contributory factor, for example prolonged kneeling in manual jobs such as a mechanic or carpet fitter.
A family history of osteoarthritis also increases the risk and so genetics are thought to be involved.
Signs and symptoms of osteoarthritis include pain and stiffness around affected joints, limited range of movement and joint instability or weakness in surrounding muscles. Exercise aimed at improving and managing arthritis is therefore often planned to help alleviate such issues. Other signs and symptoms include inflammation, a crunching or creaking sensation when moving the joints and joint deformity. Due to the impact of the condition on lifestyle and limitations to mobility, osteoarthritis can also contribute to feelings of helplessness, anxiety and depression and so mental health is a key consideration. Exercise can help to support positive mental health and can also help with healthy weight management which can also reduce the physical symptoms of osteoarthritis.

Treatment for osteoarthritis will vary based on each individual and the results of tests such as X rays and physical examinations. Medication may be used to reduce pain and limit deterioration in joints and in some cases surgery may also be used. This blog, of course, aims to discuss exercise as a means of managing symptoms. Although certain types of exercise may not be recommended for those suffering from osteoarthritis, it’s widely encouraged to keep the joints moving. The type, frequency, intensity and duration of exercise sessions will be dependent on many factors including the severity of the condition, age, fitness levels and any other medical conditions, however the below gives some general guidelines and suggestions when it comes to exercise and osteoarthritis:
Mobility and flexibility exercises can help to maintain joint mobility and range of movement. These exercises can be done seated in their simplest form or standing and therefore weight-bearing. It’s important that individuals move within a comfortable range of movement and in a slow and controlled manner to avoid any sudden movements or overextension around joints which may cause further problems. Flexibility and mobility exercises may also be performed in water, as again this provides a none weight-bearing environment and can make movements of the joints easier and more comfortable. Yoga, pilates and tai chi as well as gentle stretching can be good options.
Strengthening exercises can help to maintain joint stability and build muscular strength around affected joints. This may have declined if physical activity levels have been limited as a result of the condition or as part of the natural ageing process. Body weight exercises can be used before adding in additional resistance, although this will be dependant on each individual and their current fitness and activity levels. As with mobility and flexibility exercises, it’s important to monitor the range of movement during strength exercises for those suffering with osteoarthritis. Isometric exercises (no or small range of movement) may also be appropriate. As above, strengthening exercises can be weight-bearing or none weight-bearing, for example performed in water or whilst seated. A key consideration when it comes to strength exercises for osteoarthritis is the number of repetitions performed. This should generally be in a low range to begin with and any increase in pain should be monitored following exercise. The programming can then be amended accordingly. Pool, gym or home based exercise using light weights, household objects or resistance bands are just some of the options for strength work.

Cardiovascular exercise is a crucial part of any exercise programme and this is no different for those suffering from arthritis. Cardiovascular activities help to maintain the health of the heart and lungs and prevent conditions associated with these such as high blood pressure. It’s also a key component in healthy weight management. Low impact activities such as walking, cycling or pool based exercise are recommended for sufferers of arthritis. Cardiovascular exercise can be accumulated throughout the day to avoid prolonged periods of excessive movement. ‘Pacing’ should be considered, with frequent rest breaks or alternating of activities planned as necessary. An example of this could be combining or alternating seated with standing exercises, or choosing walking routes with benches for regular breaks.
Some other key considerations include:
All exercise and activities for sufferers of arthritis should be low impact as high impact work increases stress on the joints.
Vary activities to avoid repetitive strain and overuse.
Consider footwear choice for weight-bearing activities – cushioned soles or insoles can be beneficial.
Side effects of any medications should be considered within exercise programming.
Take adequate ‘active rest’ days, especially when beginning a new exercise programme. Be sure to monitor symptoms such as pain and stiffness following exercise and allow time for rest and recovery.
The information and tips contained in this blog are, as always, general guidelines and whilst they hopefully give you a starting point regarding exercise for osteoarthritis it’s important to get advice from qualified health and fitness professionals to suit your individual needs. As always, feel free to contact Mike at Hamers360fitness or Bev (details below) with any questions or comments.
Bev Meakin – Personal Trainer/Exercise Referral Officer and Complementary Therapist. Instagram @bevs_life

